Pain relief from top to toe
In OTC
Follow this topic
Bookmark
Record learning outcomes
Pain can pop up anywhere, often without warning. But it’s not just over-the-counter analgesics that can help make a difference
Across the human body, each square centimetre of skin contains around 200 pain receptors. These receptors send signals to the brain via the spinal cord through a whole intricate network of nerve fibres, so the brain can assess the threat and act accordingly. All of this happens in a split second.
Sometimes the nerves become damaged, or the brain’s interpretation of the signals isn’t accurate, which is why pain can become chronic, particularly after injury or as a result of disease. The 2017 report ‘Chronic Pain in Adults 2017: health survey for England’, published by Public Health England, found that 34 per cent of people reported some level of chronic pain – a figure that was unchanged from 2011.
As this suggests, pain can be caused by internal or external factors and can be short lived or stay with someone for life. From the head to the toes, wherever pain decides to manifest, pharmacy teams can be ready with a whole host of management and treatment options, lifestyle advice and preventative measures to help.
The head
Migraine is a common condition thought to affect one in seven people. It is estimated that the UK population loses 25 million days from work or school each year because of migraine, according to The Migraine Trust.
For many people, migraine is a severe headache that causes pain on one side of the head, but the symptoms are varied and complex. The frequency of a migraine attack can differ from years between migraines to some people suffering multiple attacks a week and they can last anywhere between four and 72 hours in length.
The two most common types of migraine are:
- Migraine with aura: thought to affect 10-30 per cent of people with migraine, warning signs occur before the migraine, which often include visual disturbances such as seeing flashing lights, blind or coloured spots and tunnel vision. Some people may also experience numbness, weakness, dizziness and pins and needles before a headache ensues – this can be mild or may not even occur
- Migraine without aura: the most common form of migraine, this affects 70-90 per cent of people with the condition. There are no pre-warning signs and symptoms include a throbbing headache on one side of the head, sickness, diarrhoea and sensitivity to light and/or sound.
Pharmacy teams can recommend over-the-counter (OTC) pain relief and lifestyle advice to reduce pain and prevent migraine attacks. “In terms of a treatment that is specifically for migraine, other than painkillers, there is a group of medicines called the triptans and they were designed to stop a migraine attack once it has started,” says Una Farrell, a spokesperson for The Migraine Trust. “There is one that is available over the counter – it’s called sumatriptan. There is a very specific criteria of people who can be given it: anyone over the age of 18 but under 65, and it can’t be given to patients with epilepsy, high blood pressure, kidney or liver disease.”
People with severe migraines may need to visit a GP for prescribed medication.
The condition is thought to be genetic and certain triggers are more likely to induce an attack. These include menstruation, stress, tiredness and certain food and drink such as coffee and chocolate. “We don’t know why people get migraines, but many people have triggers and some of that can be managed,” says Una. “Certain things such as if you have got a lot of change in your life – stress – can be a big trigger. Pharmacy teams can advise people to have a migraine diary; it’s a good way to understand how frequently you’re having migraines, understand the types of symptoms and what might be trigger an attack. So, if a person does have to go to a GP, they have got that extra knowledge.”
Signposting suggestion: The Migraine Trust – keeping a migraine diary.
The UK population loses 25 million days from work or school each year because of migraine
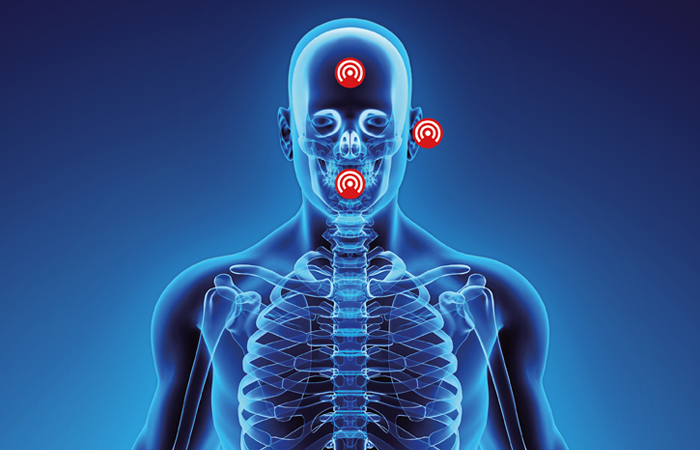
The ears
Earache can be caused by minor ear infections, but it is also potentially linked to a range of other issues, which is why it is so widely experienced. Pharmacy teams can help initially identify causes through other symptoms that occur alongside earache.
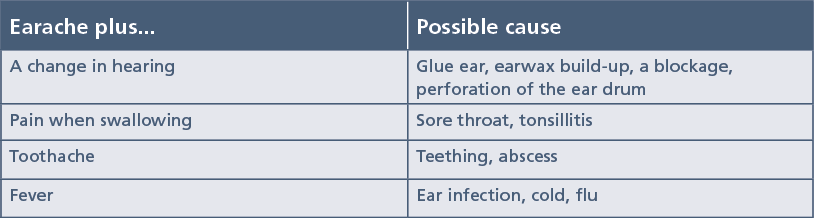
Customers may complain of a consistent or infrequent pain in one or both ears, which they may describe as dull, sharp or even burning. Earache usually clears up on its own without treatment, but pharmacy teams can recommend OTC painkillers such as paracetamol or ibuprofen to manage pain if necessary. Avoiding getting the ear wet and holding a warm or cold flannel to the outside of the ear can also help to ease the pain.

The teeth
With the doors of many dentists shut or them taking emergency patients only as a result of the Covid-19 pandemic, customers may come into the pharmacy looking for dental care, especially when there’s pain involved. Tooth decay, an abscess, a damaged or cracked tooth, a broken filling, issues with braces and infection can all cause toothache.
Customers can be recommended painkillers such as paracetamol or ibuprofen and/or a pain-relieving oral gel containing ingredients such as benzocaine where appropriate. They should also be advised to try to eat soft foods and rinse the mouth with salt water. Food and drinks that are particularly hot, cold or sweet should be avoided, as should smoking.
Some top tips to help to prevent toothache – in addition to regular check-ups at the dentist – include reducing consumption of sugary foods and brushing the teeth twice a day for two minutes with the appropriate fluoride toothpaste. For adults, toothpaste should contain 1,350-1,500ppm of fluoride. Flossing or using an interdental brush between meals can also help keep the teeth clean and prevent further problems occurring.
If a toothache has lasted for longer than two days, doesn’t ease with painkillers, or if the customer has a high temperature or a swollen cheek or jaw, they should be referred to a dentist.
Signposting suggestion: Oral Health Foundation.
The stomach
Stomach ache should not usually be a cause for worry. It can happen for myriad reasons and usually lasts for a short period of time. Some causes include:
- Trapped wind: passing wind is a very normal bodily function, with the average person releasing wind five to 15 times a day. Sometimes gas can get ‘trapped’ and cause a stomach ache so pharmacy teams can recommend OTC medication such as charcoal tablets or simeticone. Some preventative measures include avoiding certain foods that are difficult to digest, eating smaller and more frequent meals, taking regular exercise and eating and drinking slowly
- Indigestion: can cause flatulence, heartburn, bloating and feeling sick. Pharmacy teams can recommend proton pump inhibitors such as omeprazole and esomeprazole and antacids such as calcium carbonate to help ease symptoms and relieve pain. Ibuprofen and aspirin are thought to make indigestion worse, as can smoking, eating close to bedtime, and having rich, spicy and/or fatty foods. Customers should try to avoid caffeine, alcohol and fizzy drinks. Sleeping with the head and shoulders propped up may also help
- Constipation: is occurs when someone has been unable to pass stools less regularly than normal, or less than three times a week; the stool is hard, dry and lumpy; or the person is straining or in pain when passing stools. It is often caused by insufficient dietary fibre, but can be caused by a lack of fluids or exercise, or as a side effect to some medicines. OTC laxatives can be recommended where appropriate, and customers should be advised to increase their fluid and fibre intake and do gentle exercise
- Diarrhoea: can cause dehydration, fever, loss of appetite and stomach cramps, but its main symptom is the passing of frequent and watery stools. Because of this, it is important to stay hydrated by drinking plenty of fluids, pharmacy teams can also recommend oral rehydration salts if needed. Anti-diarrhoeal treatments such as loperamide can help to slow down bowel movements in adults and children over 12 years of age, where appropriate
- Food poisoning: this usually passes without treatment after a few days, but can cause a variety of symptoms such as stomach cramps, sickness, diarrhoea and a high temperature. It is often a result of food being contaminated with germs by being stored or cooked incorrectly or not reheated properly. Customers should try to keep hydrated and eat plain foods such as rice or toast.
Sudden and severe pain in the stomach can be much more serious and customers should be advised to visit a GP or call NHS 111, particularly if they are also experiencing the following red flag symptoms:
- Stomach ache that will not go away or comes back despite treatment
- Recurrent constipation or diarrhoea
- Losing weight without trying
- Blood in the stools.
A monthly pain
Period pain, also known as dysmenorrhoea, affects approximately 80 per cent of women at some stage in their life, according to the charity Women’s Health Concern. Cramps and pain can often be felt in the stomach, back and thighs. Pain usually last between 48 and 72 hours, and is usually more intense when bleeding is at its heaviest. Pharmacy teams can recommend ibuprofen, which is thought to be more effective than paracetamol for this type of pain. Applying heat to the area with a hot water bottle, or taking a hot bath or shower can help to relieve the cramps. Although exercising is often avoided at this time, it is actually thought to help reduce pain, especially swimming and walking.
The back
Four out of five people are thought to experience back pain during their lives, and it can cause severe discomfort and be extremely distressing.
There are many things customers can do to relieve back pain, and lifestyle measures are thought to provide greater longevity for easing pain than relying on OTC products such as paracetamol and ibuprofen. “[Analgesics are] really just to get you over acute episodes,” says Dr Anthony Ordman, consultant in pain medicine and advisor at the charity BackCare. “If it’s not getting better within a week then see a physio or GP.”
In terms of preventing and relieving back pain, Dr Ordman has the following advice for pharmacy teams to pass onto customers:
- Keep at a healthy weight
- Exercise weekly. “Keep the muscles that support your spine fit through regular walking and maybe doing an exercise class, something in the gym or a sport. The back depends on its muscles – they are called core stability muscles – to support it. And if they are weak, then your back is likely to get strained and painful,” he says
- Have physiotherapy when necessary
- Sit in a sensible, comfortable chair and position if sitting at a desk all day
- Avoid lying down when there is pain. “Then your muscles get weaker and get worse. Maybe take it easy for a few days and then try getting back to normal,” Dr Ordman adds.
In most cases, back pain gets better over time. By asking the right questions, pharmacy teams can help to eliminate more serious conditions such as bone, kidney or spine problems. “The first thing is not to miss anything serious,” says Dr Ordman. “[Pharmacy teams] will want to know how long the person has had [back pain]. Are they unwell? Do they have a temperature? Do they feel ill? Is it very severe pain? Because I think if you have had back pain for more than six weeks and it’s not shifting then they may want to talk to their GP about it, particularly if there is a history of cancer, or they are an older person. Or even a younger person with no history of injury.”
Signposting suggestion: BackCare.
Simple exercises to improve muscle strength can be just as effective for pain as prescription painkillers
The joints
Approximately 10 million people in the UK have some form of arthritis, according to the charity Arthritis Action, and the condition is considered to be the most common cause of disability in the UK.
Arthritis is an inflammation of the joints that can cause pain, tenderness and stiffness. This can restrict movements of the joints and lead to weakness and eventual wasting of the surrounding muscles. “People with arthritis can experience both acute and chronic pain,” says Heather Baumohl-Johnson, clinical hypnotherapist and Arthritis Action’s director of member services and operations. “This pain can make people feel low or depressed, especially if it is difficult to perform usual activities or keep up with family or friends. Managing and decreasing this pain can have a huge effect in breaking this vicious daily cycle and helping people with arthritis to live fuller, happier lives.”
There is no absolute cure for arthritis, but painkillers such as paracetamol and anti-inflammatory medicines may be recommended to help manage stiffness and pain. “These can be taken when needed or before activity that you know can trigger the pain,” says Dr Wendy Holden, consultant rheumatologist and medical adviser for Arthritis Action. “Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen can be very effective for helping pain and stiffness, but they should be used in the lowest possible dose for the shortest possible time as they can increase the risk of irritation of the stomach including ulcers, as well as cardiovascular disease, heart attack and stroke.”
Pharmacy teams can also recommend lifestyle advice to help people manage and prevent flare-ups. “Simple exercises to improve muscle strength can be just as effective for pain as prescription painkillers,” Dr Holden explains. “Exercising can also help improve balance and function, keeping people independent and sometimes delaying the need for surgery for much longer.”
Keeping to a healthy weight and eating a healthy diet can also be useful, as can relaxation methods such as meditation, which can also help to reduce any associated stress and sleep problems. Some individuals may benefit from physical therapies such as physiotherapy, osteopathy and chiropractic treatment.
Signposting suggestion: Arthritis Action.
Protect wth PRICE
Not all pain originates from inside the body; some pain occurs due to external factors such as exercise. Knowing some simple first aid techniques can be beneficial in helping with this form of pain.
Wrists, elbows, knees and ankles are susceptible to sprains, which is an injury to a ligament that supports a joint. A strain is an injury to a tendon or muscles. Pain will occur around the joint, alongside swelling and inflammation. To help reduce pain, pharmacy teams should remember the PRICE technique:
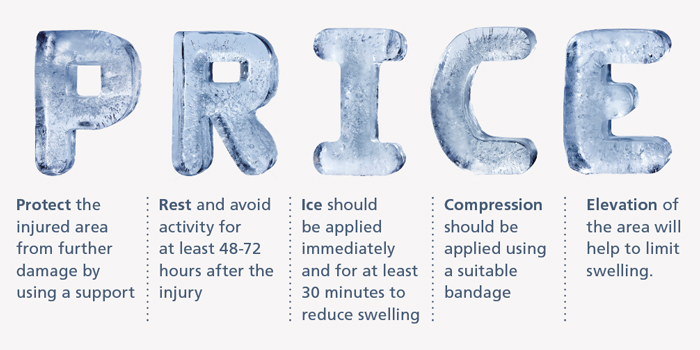
Painkillers such as paracetamol will ease the pain and ibuprofen can help to bring down swelling, although this shouldn’t be taken in the first 48 hours after an injury as it may slow down the healing. Topical products such as creams and gels are available to help ease the pain, some of which have soothing heat or cooling properties.
If the pain and swelling gets worse or doesn’t respond to treatment, referral to NHS 111 should be advised.
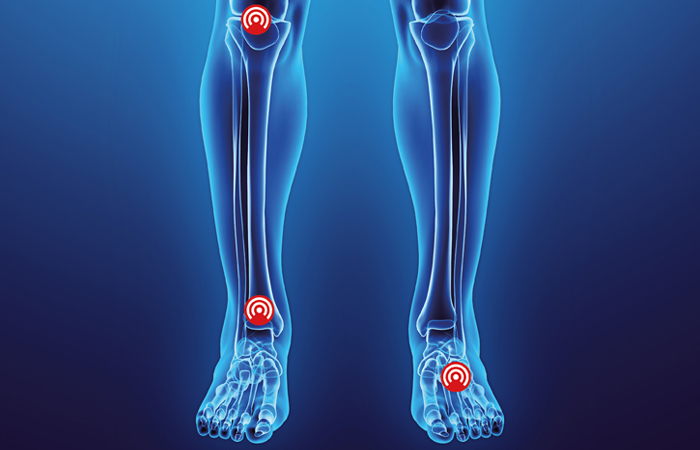
The toes
Breaking a toe shouldn’t have to warrant a trip to the hospital, and neither should an ingrown toenail; customers should be able to get the help they need from a pharmacy so they can self care.
If it is painful to put weight on a toe, or it appears to be swollen or bruised, it could be broken. Whether it’s broken or not, the treatment is largely the same and can be looked after at home, usually healing within four to six weeks. Customers can be advised to rest and raise the foot, applying ice to the area for 20-minute periods, two to three times a day. Wearing comfortable shoes and strapping the toe can also help. A broken toe should be strapped with a piece of gauze or cotton wool between the affected toe and its neighbouring one, which should then be taped together.
If the big toe is affected, a bone is sticking out of the foot, a toe is pointing at an unusual angle or there appears to be no wound on the toe, the customer should be referred to a GP or NHS 111 for further investigation.
Ingrown toenails can be very painful and painkillers such as paracetamol or ibuprofen can be taken as a starting point. The foot with the affected nail should be soaked in warm water three to four times a day for a few days to soften the skin around the nail and prevent the nail growing further into the skin. It is important that customers dry the foot well afterwards. The nail should be left to grow out itself, unless it starts to show signs of infection, in which case referral to a GP is required. If they have diabetes, they should be referred immediately to the GP as having this condition means an individual is at a much greater risk of developing foot problems and the healing process can be more complicated.
To prevent ingrowing nails reoccurring, customers should cut the nails straight across, not cutting them too short, and avoid wearing tight shoes.