Tummy talk
In OTC
Follow this topic
Bookmark
Record learning outcomes
Coeliac disease and IBS often go undiagnosed or misdiagnosed, leading to continuous discomfort and repercussions for overall health. How can pharmacy teams help customers get the correct treatment?
The gut is the one part of the body that rumbles and grumbles when it’s unhappy, due to anything from hunger and butterflies to the more serious digestive problems like coeliac disease and irritable bowel syndrome (IBS). So why is it that so many people are not talking about the only part of the body that talks back?

A reluctance to discuss bowel-related symptoms is part of the reason why – according to charity Coeliac UK – only 30 per cent of people with coeliac disease are diagnosed. And with the condition thought to affect one in every 100 people, it’s not an insignificant number of people who are suffering in silence.
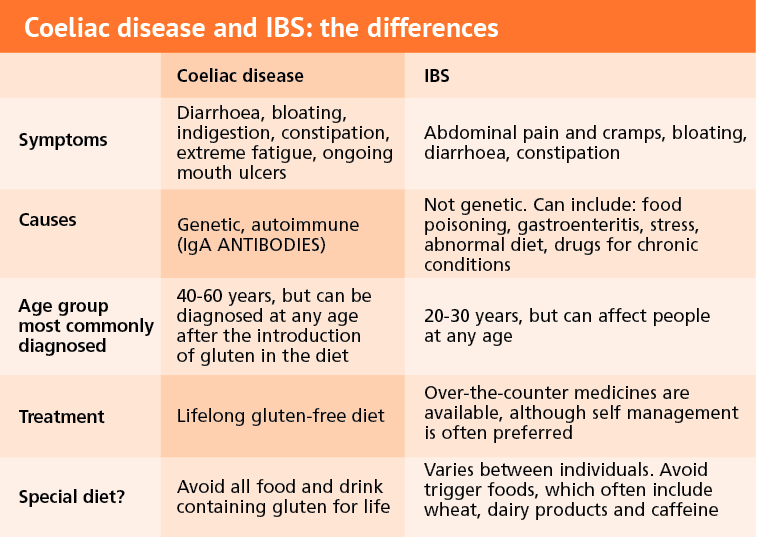
Lack of diagnosis isn’t the only issue facing those with gut problems. Misdiagnosis is also common, with one in four people with coeliac disease being incorrectly treated for IBS instead. Although the symptoms of coeliac disease and IBS are similar, the two conditions have many distinctive differences and it is important that these are recognised.
According to Coeliac UK, only three per cent of British adults are aware that the symptoms of IBS are also common symptoms of coeliac disease. Pharmacy teams can play an important role in reiterating the importance of having a correct diagnosis and informing customers that these two gut related issues can have similar symptoms but need different treatment.
What is coeliac disease?
Coeliac disease is an autoimmune condition that has a genetic basis. According to the NHS website, the chances of having coeliac disease are 10 per cent higher for those with family members with the disease, and identical twins have a 75 per cent chance of both developing it if one of the twins has the condition.
When someone suffers from coeliac disease, their immune system reacts abnormally to gluten, which is found in wheat, barley and rye, when eaten, which causes inflammation to the lining of the gut and can affect other parts of the body.
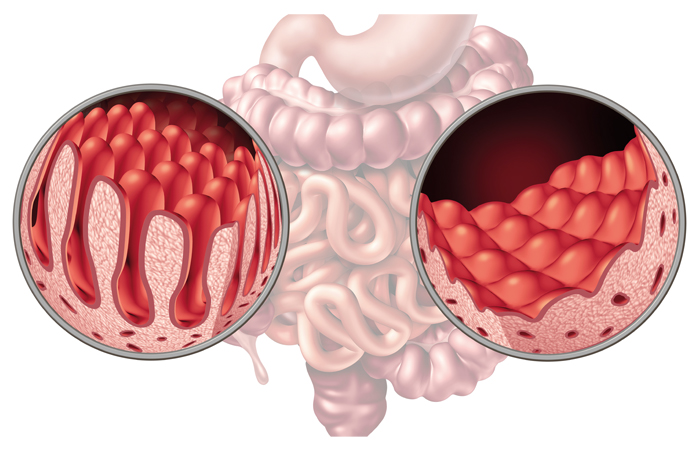
Gluten damages the lining of the gut, causing flattening of the small, finger-like villi – projections of the lining of the small intestine where nutrients from food are absorbed, resulting in malabsorption of nutrients.
Symptoms of coeliac disease can vary depending on the individual, but often include bloating, diarrhoea, nausea, wind, constipation, tiredness, anaemia, mouth ulcers, sudden or unexpected weight loss and skin rash, called dermatitis herpetiformis (DH). DH affects one in 3,300 people, according to Coeliac UK, appearing in red raised patches with blisters that may burst if scratched. The condition can develop anywhere on the body, but is often found on the elbows, knees, forearms and buttocks.
Diagnosis and treatment
Coeliac disease has a clear diagnostic process, which starts with having blood tests that detect antibodies specific to coeliac disease, in primary care, followed by referral to secondary care for endoscopy with biopsy, if the blood test is positive. Once diagnosed, the treatment for coeliac disease is to maintain a strict gluten-free diet for life.
It is vital that gluten is not removed from the diet before getting tested, according to Julie Harrington, CEO of Guts UK –
a charity committed to fighting all guts diseases. She says: “What people do is self diagnose and think ‘I’ll cut gluten out of my diet’. They do that and then they go to get tested and that’s no good because the test is irrelevant because there is no gluten in their diet.”
Once tests have confirmed coeliac disease as a diagnosis and gluten has been removed from the diet, the villi will recover and absorption of nutrients from food will improve. Norma McGough, director of policy, research and campaigns at Coeliac UK, says: “When you remove gluten completely from the diet then the symptoms will subside and you’ll start to feel better very soon and the gut will heal. The healing of the gut may take longer, it can take up to five years.”
Help from a dietitian is recommended for people with coeliac disease and IBS. “Dietitian’s are the healthcare professionals who are best placed to support people managing their gluten-free diet. Knowledge around the gluten-free diet that relates to their individual circumstances is key because this is a lifelong condition that requires lifelong dietary management,” says Norma.
Even though coeliac disease has a diagnostic test and effective treatment, the average length of time taken for someone to be diagnosed with the disease from the onset of symptoms is 13 years, according to Coeliac UK. Many people remain undiagnosed, or wait too long for a diagnosis. Julie says: “Too many people are suffering in silence. 56 per cent of people, who are struggling with gut issues, wait between six and 18 months before going to see a doctor.”
With one in four also being misdiagnosed with IBS, there is a large percentage of those with coeliac disease receiving no, or the incorrect, treatment for the condition. Pharmacy staff can help and play a key role in recognising the symptoms of coeliac disease and encourage people to visit a GP to have an initial blood test.
Help from a dietitian is recommended to people with coeliac disease and IBS
Complications
“One of the most common complications for adults diagnosed with coeliac disease is low bone density or osteoporosis and this is due to chronic malabsorption of calcium. Another very common nutritional deficiency that is diagnosed is anaemia, due to iron deficiency,” says Norma. Once diagnosed and treated with a gluten-free diet, gut healing enables absorption and improvements in bone density and anaemia. If coeliac disease isn’t diagnosed and goes untreated, there is an increased risk of ongoing complications including osteoporosis and in rare cases, small bowel cancer and neurological conditions such as gluten ataxia and peripheral neuropathy.
Gluten be gone!

Although gluten can often affect those with IBS, it is the main trigger for coeliac disease, but what is it?
Gluten is a general name for the proteins found in wheat, rye and barley, which helps foods maintain their structure and acts as a glue that holds them together.
It can be found in foods such as bread, pasta and cereals and flours, but also foods that may be less obvious such as soup, soy sauce, beer and stock cubes.
There is an increasing number of gluten-free substitute foods, e.g. breads and flour based products in retail, as well as a greater awareness in catering outlets. The National Institute for Health and Care Excellence (NICE) has created a list of gluten-free alternatives. It should be noted that many of these products have a high sugar content and customers should be advised to check the packaging before purchase.
What is IBS?
Irritable bowel syndrome (IBS) is most common in those between the ages of 20 and 30 and is thought to be twice as common for women than men. According to the Irritable bowel syndrome in adults 2017 report by the National Institute for Health and Care and Excellence (NICE), it is estimated that between 10 and 20 per cent of the population suffer from IBS.
Unlike coeliac disease, IBS is not a genetic condition. There is no specific cause for IBS and triggers vary between individuals. Some of the most common risk factors are: an attack of gastroenteritis, a traumatic or upsetting event that causes stress and courses of powerful antibiotics.
According to Guts UK, approximately one third of people with IBS have symptoms of constipation, while another third have symptoms of diarrhoea. Other IBS symptoms vary and can include:
- Bloating
- Cramps
- Frustrated defecation – needing to go to the toilet but not being able to
- Tiredness
- Nausea
- Heartburn and indigestion
- Backache
- Incontinence.
IBS manifests differently in different people, with some symptoms more prominent than others. Julie says: “IBS is irritable bowel syndrome and the syndrome is a mixture of symptoms which are all different for everybody. Some people get IBSC which is constipation, some get IBSD, diarrhoea, and some people get IBSC and D.” Pharmacy staff should be aware that treatment for IBS varies between customers. Julie adds that pharmacy staff should encourage people to get tested for coeliac to check it isn’t the disease and then establish the best treatment plan for them.
Unlike coeliac disease, an endoscopy test will not pick up on IBS because the gut is not affected in the same way. “The villi look normal but the function of the bowel is abnormal”, says Dr Simon Smale, gastroenterologist and medical adviser to the national charity, The IBS Network, adding that when comparing the two conditions, “one is a problem with the way in which the gut moves [IBS] and one is a problem with the way in which the surface of the gut functions [coeliac disease].”
Simon adds that pharmacy staff can play a vital part in diagnosis. “IBS is a clinical diagnosis made on the basis of the story people tell and having excluded other conditions.”
IBS manifests differently in different people
IBS treatments
Just as there is no diagnostic test for IBS, there is no universal treatment. However, pharmacy teams can be on hand to reassure customers that there are viable options to help manage their condition and help them find a tailored, effective treatment programme for their individual symptoms. For example, someone suffering with symptoms of constipation will have a different treatment plan to someone suffering from diarrhoea.
-
Dietary management
Identify trigger foods that cause IBS symptoms by keeping a mood and food diary. This this can be easily recommended by pharmacy staff and can help to pinpoint certain trigger foods, making a significant impact.
Simon says: “I would start with dietary intervention. Eat small meals often, rather than all your calories in one large meal at the end of the day. Avoid caffeine, alcohol, fizzy pop and indigestible complex carbohydrates.” Lifestyle is also important and those with IBS should ensure they take time to relax and achieve the recommended levels of exercise. “Don’t ignore the impact of lifestyle, sleep is important and getting good quality sleep has a significant impact on the way the gut functions,” Simon adds.
Other things customers with IBS should avoid include:
- Skipping meals
- Drinking more than three cups of tea or coffee a day
- Eating more than three portions of fresh fruit a day
- Eating processed, fatty or spicy food
- Eating quickly.
If customers suffer from constipation, fibre and bulking agents like natural bran, a natural laxative, can help but may increase abdominal pain slightly in some people.
-
Low FODMAP diet
A FODMAP diet is the exclusion of fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP), which are complex sugars that are not easily absorbed. They are found in a variety of fruits and vegetables, milk and wheat. As with treatment for coeliac disease, pharmacy staff should recommend that the decision to follow special diets, especially exclusion diets like the FODMAP diet, should be supported by a dietitian.
-
Drug therapy
Rates of successful drug treatments for IBS are relatively low. Simon says drugs usually only help around a quarter of customers, with an eighth suffering from side effects. A variety of drugs are available over the counter (OTC) that target specific symptoms of IBS, and drugs to treat constipation and diarrhoea – such as laxatives and loperamide respectively – could be recommended.
-
Probiotics
These are thought to help restore the balance of bacteria in the gut. The NHS recommends that people with IBS can try taking probiotics for about a month to see if they help ease their symptoms. Julie says pharmacy staff should suggest probiotics, where appropriate, commenting: “The one thing about probiotics, even the stuff that’s really readily available on the supermarket shelves, is it does no harm.”
Simon adds: “Probiotics and prebiotics have influence on gut motility, development of gut and central nervous system”, meaning their benefits are even more wide ranging.
-
Complementary therapies
Some research suggests a link between the gut and the brain, as stress can be a significant trigger of IBS in some people. As such, hypnotherapy and relaxation therapy can also be used to treat IBS, although, again, treatment success varies between individuals.
Further information
The following organisations can provide further information and support for pharmacy teams and customers:
- Coeliac UK: 0333 332 2033
- The IBS Network
- Guts UK: 020 7486 0341
- NHS: coeliac disease / IBS
